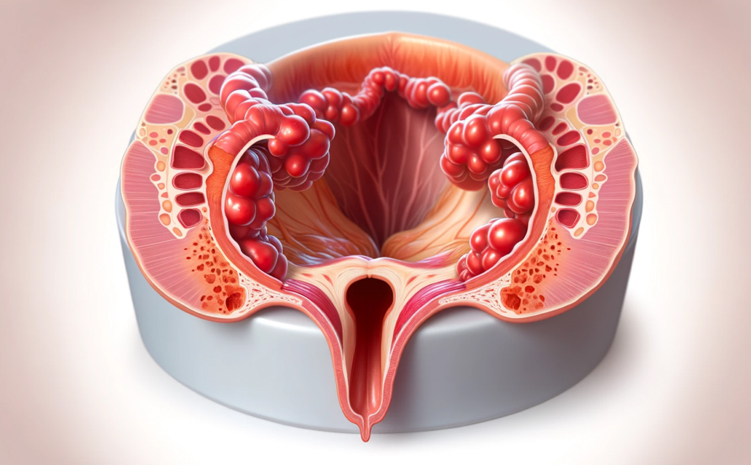
Anal fissure disease is the cracks that occur in the skin part called anoderm at the entrance of the anal canal, which is the last part of the large intestine. These cracks anatomically extend between the sawtooth-shaped border of the anal canal, called the dentate line, and the anal edge entrance, called the anal verge. These cracks do not exceed the upper limit of the dentate line. The length and depth of these cracks in the outer part of the anal canal may vary from case to case and even at different times in the same case.
Anal fissure is typically seen in locations in the anal canal where blood flow is least and tension during defecation is greatest. The majority of them (about 90%) are localized in the posterior midline. Rarely, they may develop in the anterior midline. Although it is seen equally in both genders, only 1% of the anal fissures seen in men are located in the front, while this rate is 10% in the female gender.
Anal fissure disease can be seen in all age groups (the most common cause of rectal bleeding in babies is acute anal fissures). However, it is an important health problem of the young adult population.
What is the Frequency of Anal Fissure in the Society?
Although the prevalence of anal fissure disease in society cannot be determined due to misinterpretations of patients' complaints about anal health (attributing most of their anal-related complaints to hemorrhoidal diseases), physician deficiencies in terms of diagnostic criteria, and inadequacies in the recording system, the predominant opinion is that it is one of the most common anectal problems.
What Causes the Formation of Anal Fissures?
Clinically, fissure development almost always occurs following chronic constipation (long-term constipation) and/or a difficult stool passage (straining during defecation). Here, it should be kept in mind by the physician and the patient that anal fissure disease, which occurs as a result of the complaint of constipation, which is the main factor in the formation of anal fissure, may actually be the visible part of the iceberg and that there may be another and more serious health problem underlying the etiological cause. The key points in the findings and history should be evaluated by the physician. Further examination may be required when deemed necessary.
The reasons for the emergence of the disease were revealed by examining anal manometric (measurement of anal canal pressure), arteriography and laser doppler findings.
In the light of these studies, we now know that the two prominent factors in the pathogenesis of anal fissure disease are internal anal sphincter hypertonicity (excessive increase in the tone and pressure of the internal muscles surrounding the anus) and lack of blood supply in the posterior midline. The main principle in the treatment of anal fissure disease focuses on eliminating IAS spasm (reducing internal muscle pressure).
An important point that is still debated and not clearly explained today is whether this increase in muscle pressure develops initially or is a secondary result triggered by the pain symptom associated with the disease. Patients postpone their toilet needs due to severe pain in the anus, and this causes the stool to harden and defecation becomes more difficult over time. As a result, the current situation creates a vicious circle. In order to break this cycle, the treatment aims to reduce muscle pressure to ideal levels and increase blood flow and wound healing in the fissure line with the methods we will explain later.
There are cases where anal fissure develops without constipation. Fissures do not develop in every patient with long-term constipation. In addition, the absence of IAS spasm in some patients, which is a very important patient group, and even patients with anal fissures with low sphincter pressure cannot be explained and their treatment may be difficult.
What are the Clinical Symptoms and Signs of Anal Fissure Disease?
The leading sign and symptom of anal fissure disease is severe pain provoked by defecation. Especially when examined by the physician, the patient describes this pain as "tearing" and "like pulling out a small piece of glass". By questioning this pain definition well, it is possible to reach the diagnosis of anal fissure almost completely at the anamnesis (story) stage. Bleeding is usually minimal. It is not uncommon for patients to report no signs of bleeding. Bleeding on the floor of the fissure, noticeable on toilet paper, is almost always secondary to hemorrhoidal disease.
It should not be forgotten that there is a possibility of an "iceberg phenomenon" (the visible part of the iceberg) in the clinical picture of anal fissure. For example, rectocele (intestinal hernia) disease may be underlying the constipation that causes fissure.
An important and important point that should be emphasized is that there is no typical pain complaint and that atypically located fissures (located differently from the standard localization of the posterior midline and anterior midline) detected by the physician during anal examination should be investigated in detail. It should not be forgotten that anal region diseases are interrelated in terms of the symptoms of the disease, and in cases, fissure may occur with concurrent hemorrhoidal disease. Therefore, it is possible to detect a fissure associated with hemorrhoidal disease in a patient presenting with a secondary bleeding symptom in the fissure.
It should also be kept in mind that in chronic anal fissures, there may be skin folds on the fissure floor, which will be explained in detail, which may be felt by the patients and may cause the patients to perceive that this is a hemorrhoid pack.
How to Classify Anal Fissure? Why Is This Difference Important?
Anal fissures are classified as acute, chronic, and sometimes typical and atypical fissures. It is important to determine and record in the clinic whether the fissure is an acute anal fissure (acute AF), chronic anal fissure (chronic AF) or atypical fissure.
Acute anal fissures are superficial cracks with a short-term history. They can develop after constipation and sometimes diarrhea attacks in all age groups, including babies. The lesion is not deep. During the anal examination (it is a fact that the patient may feel severe pain, even during the separation of the hips during the examination, and this group of patients may move away from the treatment. The patient-physician relationship is very important in this sense, to reassure the patient who is already anxious due to the anal examination.) It resembles being scratched with a scalpel. With appropriate conservative treatment, they usually heal within 4-6 weeks.
Chronic Anal fissures are deep and persistent lesions. It is possible to see internal muscle fibers on the floor of the crack. The existing opening due to the crack is swollen around the lesion as a result of long-term inflammation. In some cases, it may cause the development of skin folds called skin tags. With a similar mechanism, a hypertrophic papillae appearance into the anal canal can also be detected. (Patients may perceive these lesions as hemorrhoids, and it is inevitable that they will end in absolute failure if they seek results with hemorrhoid medications based on their own diagnosis.) According to clinical definitions, pain symptoms lasting longer than 6-8 weeks are included in the diagnosis of CAF.
Rarely, the base of the fissure is infected and an anal abscess (anal abscess) may develop as a result of a superficial fistula on the basis of the existing chronic anal fissure. It is important for the physician not to ignore the underlying anal fistula in these patients.
Atypical fissures are fissures that develop secondary to diseases such as Crohn's, AIDS, cancer and tuberculosis. It is necessary to take into account their unusual features such as being mostly localized laterally (on both sides of the anus), being painless, and not having the normally expected spasm in the anal canal tone. These peculiar anal fissures need to be investigated in detail.
How to Diagnose Anal Fissure?
In anal fissure disease, it is possible to reach the diagnosis with almost complete accuracy at the story stage by carefully examining the typical "tearing-like" severe pain complaint described by the patient that is provoked by defecation. After a specific history of this disease, the diagnosis is confirmed by examination, preferably on a proctological table in appropriate lighting conditions. During the diagnosis phase of Anal Fissure, it is extremely important to classify the fissure as acute, chronic and atypical when it is identified, and to record the fissure localization and additional examination findings.
In this group of patients who are anxious about their sense of privacy, it will be important to talk to the patient during the examination phase to ensure that he or she is relaxed, and to inform the patient about the pain that may be felt during the manipulations to be performed while observing the anal area during the procedure. For this reason, in some patient groups complaining of pain in the anus, it is also necessary to perform anal region examination under anesthesia.
Under normal circumstances, no imaging examination is required for the diagnosis of anal fissure. However, when the severity, type and duration of the pain in the area, and the presence of additional symptoms are evaluated by the physician, it should be kept in mind that if the physician thinks that this type of pain cannot be explained by anal fissure, additional tests may be requested. Colonoscopy will not be performed routinely in this patient group, and when the cause and effect relationship is examined and it is thought that the existing fissure is actually related to other underlying disease groups, the patient can be informed and colonoscopy can be performed after the anal fissure treatment is performed and the symptoms regress.
Non-Surgical Methods in the Treatment of Anal Fissure Disease?
In the treatment of acute fissure, the patient should consult his physician as soon as possible after his current complaints and keep in mind that anal fissures can be improved with non-surgical suggestions and lifestyle adjustments. Unfortunately, patients attribute most of their existing complaints in these disease groups, where the sense of privacy predominates, to hemorrhoidal diseases. They are stuck in the density of information in their immediate environment and on the internet, causing delays in the disease with the so-called "treatment methods" they provide with their own means, and the current situation causes anal fissures to deepen. It can become chronic and even progress to an infected focus, resulting in anal abscess and anal fistula.
Classified as acute anal fissures; It is a classical knowledge that conservative treatment methods for anal fissures, which are superficial and the patient's entire history does not exceed 6 weeks, include fiber diet, hot water baths with a shower head and, when necessary, application of local anesthetic pomades to the anal area, providing a large and rapid recovery. According to literature information, up to 90% improvement has been found in the treatment of acute anal fissure with just adding bran to the diet and hot water baths twice a day. In chronic anal fissures, success rates fall below 30% with the conservative approaches listed above. Therefore, it has been accepted that more radical treatments should be applied to reduce internal muscle spasm (Internal Anal Sphincter muscle tone) in a case that has had symptoms for weeks and has been diagnosed with chronic anal fissure by an experienced proctologist.
In modern surgical practice, the treatment algorithm of chronic anal fissures has been determined based on scientific evidence with support from the literature. As will be discussed in detail in our other topics, three main treatment methods for chronic anal fissure have been determined, beyond conservative approaches: non-surgical GTN-containing ointments, botox injection application and surgical Lateral internal sphincterectomy surgery. The main target of all these treatment methods is the internal muscle groups, with the aim of normalizing the increased resting pressures in chronic anal fissure patients.
Use of Medication (Creams containing Glyceryl Trinitrate) in the Treatment of Anal Fissure Disease?
In the treatment of anal fissure, the common consensus of the European Study Group (authors of eight European countries) and the American Society of Colon Rectum Surgery is that the use of creams containing GTN should be the first step of treatment in the treatment of anal fissure. (application of non-operative treatment methods in the first step)
The main target of all surgical and non-surgical options in anal fissure treatment is to reduce the high rest pressures in the anal area by resolving the spasm in the internal muscle groups, thereby increasing the blood flow in the anal fissure and ensuring wound healing in the anal fissure.
GTN (cream with Glyceryl Trinitrate active ingredient) increases the blood flow in the anal fissure localization by reducing the pressure in the internal sphincters. While GTN relaxes the internal anal sphincters (inner muscles around the anal), it does not cause any damage to these muscle groups and its effect is reversible. Patients should be informed that it should be applied twice a day, following defecation in the morning and drying after a hot water bath, and before going to sleep at night. The important point to emphasize is that the cream should only be applied in the size of a lentil. The cream should be applied to the muscle groups around the anus without entering the anal canal.
An important point that the physician should inform the patient about when using this drug is that approximately 20-25% of patients may complain of headache during the treatment process. This pain is not resistant in most patients and can be controlled with simple painkillers. Only in about 10% of this patient group, there may be cases where the headache is persistent and the treatment must be discontinued. However, clinical improvement will be observed following drug discontinuation.
Drugs containing the active substance GTN cause relaxation in the inner muscle groups of the same anal area, as well as in the vascular walls, which are considered to be the causes of headaches, and cause the vessels to expand. For this reason, it should be used with caution, especially in patients with cardiac problems and migraine.
In the light of the literature information, the effectiveness of the active substance at 0.4% concentration has been approved and there are commercial forms of drugs containing GTN. Despite this initial effectiveness of the drug, it should be known that it has handicaps in terms of continuation of treatment and high relapse rates. Based on literature information; It has been shown that the effect of creams containing GTN on fissure healing is less than Botox and surgery. It is recommended to use the drug twice a day. After the pain disappears, the medication must be continued for 2 weeks. If treatment fails after 6 weeks, other treatment steps should be considered.
Botox Injection in Anal Fissure Treatment?
Botox injection is an important non-surgical application that has taken its place in the chronic anal fissure treatment algorithm, based on literature and evidence. The target point of anal fissure treatment in Botox injection is; By reducing internal sphincter muscle spasm (high pressure in the internal muscle groups around the anus), blood flow in the anal canal is increased and anal fissure healing is facilitated.
With Botox application, paresis (muscle paralysis) lasting for weeks is achieved in the internal anal sphincters (inner muscles around the anus). It is important to inform the patient that this effect will last for approximately 4 months, that this period is sufficient for wound healing, and that the muscle contraction feature will be regained after the effect returns. It is extremely important for both the chance of success and the risk of incontinence that the application be performed by a physician who has technical knowledge such as where the application will be made, at what doses it should be done, and how much the Botox vial should be diluted with sterile saline solution. Compliance with the cold chain should not be neglected during the transportation of Botox vials and the transfer should be ensured immediately before application with meticulous programming. The medicine is gentle in this respect. The way the vial is prepared contains some tips.
Botox has been shown to be superior to GTN-containing creams in symptomatic relief and fissure healing. The success rate of Botox injection in the treatment of chronic anal fissure reaches up to 80%. However, this rate; It is lower than Lateral Internal Sphincteratomy Surgery, which is considered the "gold standard" in the treatment of the disease today. (According to literature information, the chance of success after LIS surgery is 94-100%.)
An important piece of information that the physician should give to the patient is that recovery with Botox is slower than the surgical option. (Although there is symptomatic relief in the early period after the surgical procedure, Botox infection progresses slowly. Full recovery may take 4-6 weeks.)
Surgical Treatment of Anal Fissure Disease
In the surgical treatment of anal fissure, according to the literature results, a single operation has been decided in evidence-based modern surgery. The operation, called lateral internal sphincteratomy, provides a rapid symptomatic and objective recovery in anal fissure disease by cutting the internal muscle groups, reducing the resting pressure around the anus and increasing blood flow.
In this sense, the rapid response to anal fissure treatment after the LIS operation is superior to Botox injection, which may have a slower course. In LIS surgery, which is considered the gold standard in the treatment of anal fissure, it has been a matter of long-standing debate on which location the muscle groups will be cut, but later on, a common consensus decision was made to perform the procedure from the lateral, i.e. outer, part of the anus, where blood supply and therefore wound healing are best. Apart from this issue, which is still discussed by the authorities, another issue that is still discussed by the authorities today is how much muscle group will be cut. Two different anatomical localizations have been described in two different views. As a result of these discussions, our clinic's opinion is that the ideal sphincterotomy can be performed with a gradual incision and appropriate pressure and calibration measurements to ensure the normal pressure or calibration targeted for each patient.
In the operation defined as spasm-controlled sphincterotomy, a gradual sphincterotomy strategy should be applied until each patient's anal calibration (the limit of advancing a blunt cylinder into the anal canal without difficulty) reaches the diameter of 29-30 mm in normal adults. With this controlled strategy, according to literature information; The rates of both recurrence and deterioration in anal continence (ability to hold gas and stool) have been reduced. The surgery in which this controlled cut is made by taking pressure measurements is called pressure-controlled sphincterotomy.
The success rate of LIS surgery, which is the gold standard in the treatment of anal fissure disease, is 94-100%. The physician must inform the patient in detail about complications of the surgery, such as bleeding, hematoma (blood accumulation), abscess, and fistula, which occur in 7% of cases. (It is important to know that these figures belong to physicians experienced enough to publish case series, and that these rates are significantly higher since they are performed in random centers. The most important and serious complication of LIS is incontinence. Although it is minimal and temporary most of the time, this rate is 45%. According to research, it can be up to 1.2% and may affect the patient's quality of life.
As a result of all this evidence-based scientific data, it is extremely important that these operations be performed in the operating room environment (we do not recommend that they be performed in the office environment) by physicians who are familiar with the diseases of this region and are experienced.
If the patient is at the center on the morning of the surgery and the pain is controlled in a controlled manner, the patient will be taken into operation after an anal enema. There is absolutely no need for the patient to receive general anesthesia for this operation. It is an operation with a planned surgery duration of approximately 2 minutes, with superficial sedation performed by an anesthesiologist and local anesthesia support from the surgeon. Bleeding control is extremely important here. There is no harm in discharging the patient after a few hours of follow-up. He will be called for a follow-up examination the next day.
In the postoperative period, postoperative recommendations for all perianal region diseases and an appropriate diet program, which is extremely important in preventing the disease, will be given. Correct toilet habits of patients is an issue that should be emphasized. The patient will be advised to take water baths in the anal area with a hot shower head after defecation in the morning without straining.
Special Group of Patients with Anal Fissure
Increased anal canal pressure, which is an extremely important feature of anal fissure disease and a common feature of the majority of cases, is paradoxically not present in a rare group of patients. In other words, in these patients, contrary to expectations, the pressure in the anal area is not high, on the contrary, it may be normal or even low. Therefore, it would not be right to further reduce the anal pressure in such a disease group (which may occur in postpartum cracks). In these patients, special surgical options such as sliding flaps in the anal region should only be evaluated and evaluated by experienced centers. It is important to measure anal pressures manometrically in these patients before surgery.
Anal fissures are common in Crohn's patients at a rate as high as 30%. Anal fissures seen in this patient group are usually in atypical localization, deep, deformity, and sometimes occur simultaneously with anal fistula disease. Therefore, as we have mentioned before, the doctor must be careful not to miss an underlying Chron's disease in the fissures with the differences we mentioned. As with other lesions in Chron patients, surgery should be performed only in the presence of complications, because the risk of incontinence will be high in surgery in these patients. It should be kept in mind that in this group, with a multidisciplinary approach and appropriate medical treatment, anal symptoms and signs will disappear at a rate of 50% in response to the disease.
The approach to patients who have undergone LIS (previous surgery) but do not experience clinical relief is still a matter of debate. It is important that these cases are evaluated by specialist physicians. In these patients, pressure measurements should be made and non-surgical methods should be considered first.