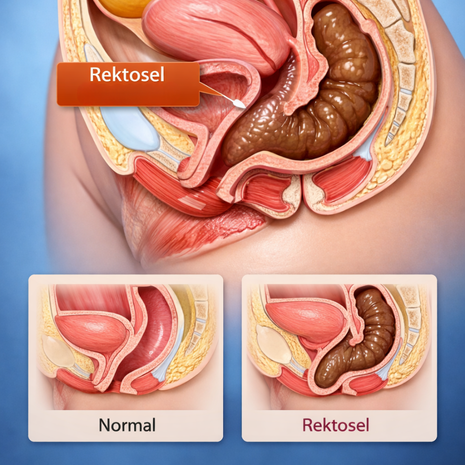
A rectocele is a pelvic floor disorder in which the rectum bulges forward into the vaginal wall due to weakening of the rectovaginal septum. It commonly affects women who have given birth vaginally or those suffering from chronic constipation. Symptoms often include difficulty emptying the bowels, a feeling of pelvic pressure, constipation, bloatingand the need to use fingers (splinting) to assist evacuation.
If untreated, a rectocele gradually enlarges and may lead to persistent bowel dysfunction, pelvic pain, sexual discomfort and reduced quality of life. Diagnosis is mainly clinical and can be confirmed by MRI defecography, which shows the bulging of the rectum during defecation.
Treatment is individualized — ranging from pelvic floor therapy and constipation management to surgical reconstruction.
What is a rectocele?
A bulging of the rectum into the vagina due to structural weakness of pelvic connective tissue
Why does it occur?
Pregnancy, childbirth trauma, menopause-induced tissue laxity, chronic straining, obesity and genetic weak collagen.
Who is most at risk?
Women >40, especially after multiple vaginal births.
Symptoms
Incomplete evacuation, pelvic pressure, vaginal fullness, constipation, bloating, splinting.
How is rectocele diagnosed?
Rectocele is primarily diagnosed by taking a detailed medical history and performing a thorough pelvic examination. During vaginal and rectal examination, the patient is asked to strain in order to assess whether the rectum bulges into the vaginal wall. To confirm the diagnosis and determine the severity of the rectocele, MRI defecography is considered the most valuable imaging method. In selected cases, pelvic ultrasound or colonoscopy may also be used.
How is rectocele treated? Are there non-surgical treatment options?
Treatment of rectocele depends on the severity of the condition and the intensity of the patient’s symptoms. In mild to moderate rectocele, non-surgical treatment options are usually the first choice. These include managing constipation, adopting a high-fiber diet, adequate fluid intake, pelvic floor muscle strengthening exercises (Kegel exercises), pelvic floor physical therapy and biofeedback therapy.
In advanced cases or when symptoms persist despite conservative treatment, surgical intervention may be required. The goal of surgery is to repair the weakened rectovaginal support tissue and restore the rectum to its normal anatomical position.
What problems can occur if rectocele is left untreated?
If rectocele is left untreated, it may gradually worsen and significantly reduce a patient’s quality of life. Common problems include worsening constipation, a persistent feeling of incomplete bowel emptying, and chronic bloating and gas complaints. In advanced cases, patients may need to use their fingers to assist bowel movements (splinting).
In addition, vaginal pressure and fullness may increase, and pain or discomfort during sexual intercourse can occur. Untreated rectocele may further weaken the pelvic floor and contribute to the development of other pelvic organ prolapses, such as uterine or bladder prolapse. Over time, symptoms may become severe enough to require surgical treatment.